Create the Optimal Healthcare Provider Network Designed for Quality Outcomes
To Build a Better Provider Network, Start with Better Data About Your Providers

There are a lot of reasons healthcare payers want to build optimal provider networks. An optimal provider network is smarter: it lets payers synthesize data from many different systems, including recruiting, credentialing, claims, reimbursements, utilization, quality, fraud detection, and more. With an optimal provider network, health plans are more competitive in a marketplace driven by changing consumer choice, population health programs, and value-based purchasing. An optimal provider network allows health plans to address network adequacy, consumer choice, and even the accuracy of insurer’s provider directories, which is critical to maintaining regulatory compliance and avoiding fines in a rapidly evolving regulatory landscape. And optimal provider networks deliver high quality care because they combine sufficient capacity and provider distribution to consistently meet the health care needs of the covered population while avoiding unreasonable delays and wait times.
Common to each of these efforts is a reliance on accurate provider information. It streamlines and accelerates critical decisions, regulatory reporting, and the patient and provider experience. But, the unfortunate reality is that reliable, trustworthy data about providers remains elusive in spite of decades of effort. To make better business decisions about which providers to include or exclude from your optimal provider network, you need trusted, relevant, and authoritative data about each provider, delivered in time to meet your business demands.

What’s in a Name?
Consider a (fictional) participating provider: Margaret Smith-Jones, MD. How do you analyze her value to your optimal provider network if she appears in your credentialing system as ‘Dr. Peggy Smith,’ but, in your claims system, her name is ‘Maggy Smith-Jones, MD’, and in your provider relations system, her name is ‘Dr. Margaret Smyth-Jones’? And what about capturing information about whether Dr. Smith-Jones has multiple specialties? How do you find out if she has multiple board certifications, or verify whether she practices at multiple facilities? When she shows up in these systems as what appears to be three different individuals, it becomes challenging to gain a single, trusted, understanding of her value to your organization.
Continuing the scenario, if you know that her NCQA scores are in the 35th percentile, you might decide that removing her from the network is your best approach to improve the quality scores for your provider network. But, would you reconsider that decision if you knew that she is the only PCP in a very rural area? You might decide to train Dr. Smith-Jones to support network adequacy rather than remove her.
However, if you knew that she’s had twelve malpractice claims, two sanctions, and one board action in the last five years; then removal from the network might actually be your better business decision. And just how do you effectively comply with the new 2019 CMS regulations for provider management, when she has three distinct personas across your systems?
A Changing Regulatory Environment
We’ve seen U.S. federal and state regulators revise network adequacy rules that have been in place for decades. Keeping pace with regulatory changes can be a daunting task for health plans, rarely delivering a sustainable competitive advantage for payers. And while federal regulators historically tended to defer to individual states to regulate provider networks, no clear national standard has emerged among the states.
Complex regulatory frameworks now abound to mandate consumer protection and manage network adequacy, such as California Timely Access to Care and New York Emergency Medical Services and Surprise Bills. This year, in 2019, CMS has already proposed and finalized multiple regulations that impact how health insurance payers must manage their provider networks. There are new rules affecting payment reassignment for Medicaid providers, along with new rules affecting claim rejection for Medicare Advantage and Part D providers on the Preclusion List. CMS has also begun proposing new rules to strengthen oversight of Accrediting Organizations, including ownership changes, provider deficiencies, and conflicts of interest.
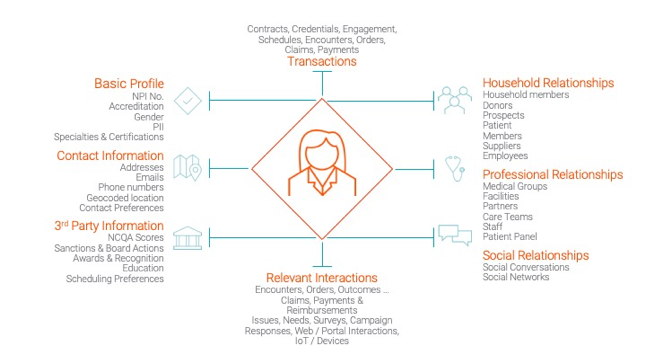
A 360° View of Every Provider
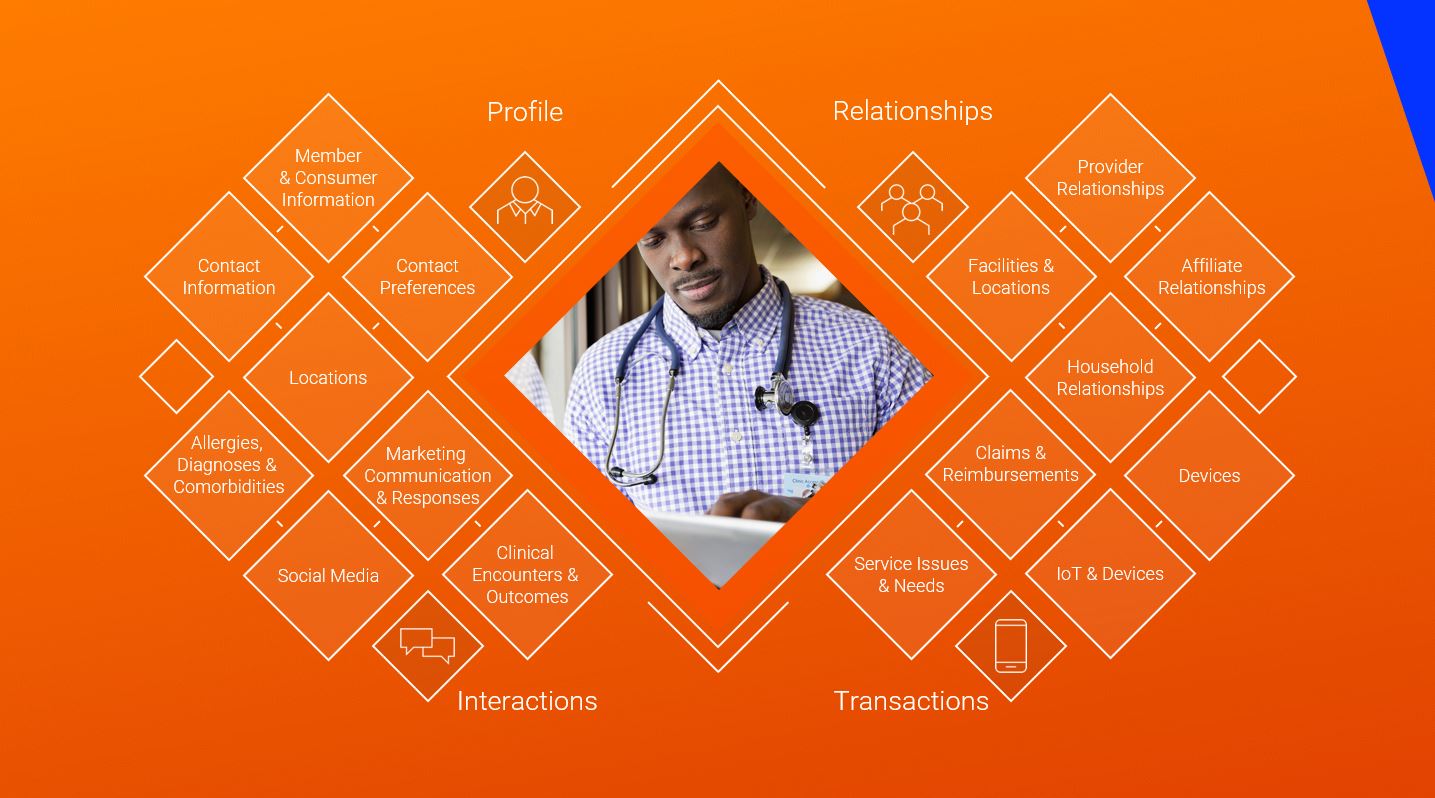
By reconciling those three personas into a single, trusted, 360 degree view of Dr. Smith-Jones, and fixing the quality of your provider data across the systems you rely on, you improve your ability to accurately measure the true cost, quality, utilization, and member experience within your existing provider network. And, not only that, you also expand your ability to drive future innovation through data-driven insights that empower you to introduce new reimbursement models, support network expansion, and develop new health plan products.
Learn more about Informatica’s solutions for payers and healthcare providers.







